Dyspraxia?
Maybe.
Parents notice things about their own children that seem a bit… off. And it can be difficult to get help – many doctors and nurses will simply shrug off a parents’ concerns as no big deal – as normal differences between children. And for most children, any one symptom of Dyspraxia is in fact, no big deal. Many kids are not diagnosed until after 3 years of age when symptoms continue to persist and developmental delays compared to their peers are clearly evident. Sometimes, a child may not be diagnosed until their teenage years.
A pediatric neurologist can confirm a formal diagnosis of Dyspraxia. However, there are things to look for as a parent before you take the step of getting a formal evaluation.
Many of these characteristics are seen at different stages in the life of every child. But dyspraxic children exhibit a continual, combination of several of these markers, as well as some new developmental delays even with intervention.
Some may exhibit only a few of these markers in each phase of growth, but as the child grows, the particular issues a parent noticed in previous stages of development will make more sense.
After you browse this list (and before you panic), read what Dyspraxia is and what Dyspraxia is not.
Sources: Dyspraxia USA, Dyspraxia Foundation UK, other.
0-3 years
- Irritable and difficult to comfort – from birth
- Delayed early motor development – does not crawl, rolls from side to side, cannot sit unaided
- Difficulty during feeding such as tongue thrust and food being pushed out of the mouth
- Sleeping difficulties: problems establishing routine, requires constant adult reassurance
- High levels of motor activity: constantly moving arms and legs
- Repetitive behaviors: head banging or rolling
- Sensitive to high levels of noise
- Continued problems with development of feeding skills
- Toilet training may be delayed
- Avoids constructional toys such as jigsaws and Lego
- Delayed language development: single words not evident until age 3
- Highly emotional: easily distressed, frequent outbursts of uncontrolled behavior
- Concentration limited to 2 or 3 minutes on any task?
- May not be able to run, hop, jump, or catch or kick a ball although their peers can do so
- Low muscle tone (hypotonia)
3-5 years
- Very high levels of motor activity:
- Feet swinging and tapping when seated
- Hands clapping or twisting
- Unable to stay in one place longer than 5 minutes
- Very excitable:
- Voice loud and shrill
- Easily distressed
- Temper tantrums
- Moves awkwardly:
- Constantly bumping into objects and falling
- Associated mirror movements, hands flap when running or jumping
- Difficulty pedaling tricycle or similar toy
- Poor ground awareness
- No sense of danger, jump from inappropriate heights
- Continue to be messy eaters:
- Often spill liquid from drinking cups
- Prefer to use fingers to feed
- Avoids constructional toys:
- Jigsaws
- Building blocks (Lego)
- Poor fine motor skills:
- Pencil grip
- Use of scissors
- Immature drawings
- Isolated in peer group:
- Prefers adult company
- Laterality still not established:
- Problems crossing mid line Language Difficulties Persist
- Children often referred to speech therapist
- Sensitive to sensory stimulation:
- High levels of noise
- Dislike being touched or wearing new clothes
- Limited Response to verbal instructions:
- Slower response time
- Problems with comprehension (due to working memory delay, not cognitive)
- Limited concentration:
- Tasks often left unfinished
- Performs better on a one-to -one basis
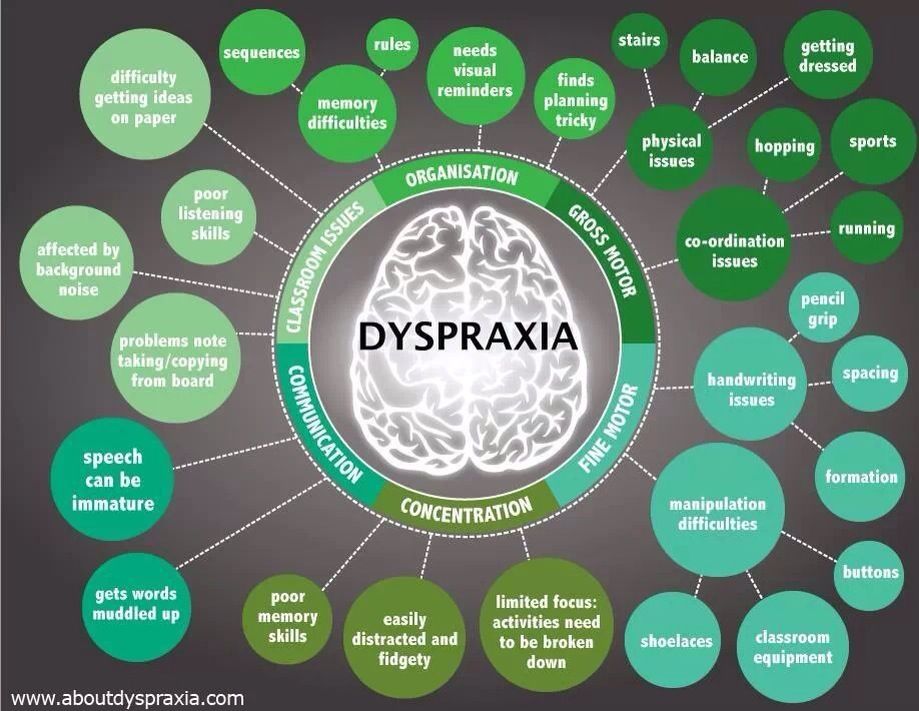
Wikipedia breaks down some of the symptoms of Dyspraxia as evidenced between fine and gross motor skills:
Gross motor control (issues):
- Poor timing
- Poor balance (sometimes even falling over in mid-step). Tripping over one’s own feet is also common.
- Difficulty combining movements into a controlled sequence.
- Difficulty remembering the next movement in a sequence.
- Problems with spatial awareness, or proprioception.
- Trouble picking up and holding onto simple objects such as pencils, owing to poor muscle tone or proprioception.
- Clumsiness to the point of knocking things over and bumping into people accidentally.
- Difficulty in determining left from right.
- Cross-laterality, ambidexterity, and a shift in the preferred hand are also common in people with developmental coordination disorder.
- Problems with chewing foods (time to chew, movement of food with tongue, etc.)
Fine motor control (issues):
- Problems using a knife and fork
- Fastening buttons and shoelaces
- Brushing teeth
- Styling hair
Handwriting issues:
- Learning basic movement patterns.
- Developing a desired writing speed.
- Establishing the correct pencil grip
- The acquisition of graphemes – e.g. the letters of the Latin alphabet, as well as numbers.
Developmental verbal dyspraxia
Wikipedia: Developmental verbal dyspraxia (DVD) is a type of ideational dyspraxia, causing speech and language impairments. This is the favoured term in the UK; however, it is also sometimes referred to as articulatory dyspraxia, and in the United States the usual term is childhood apraxia of speech (CAS). (Ed. Note: Apraxia is a very different issue resulting from brain trauma or stroke. The use of the term Apraxia of Speech is not indicative of apraxia, but a lack of a diagnosis of dyspraxia and will hopefully fall out of favor. – Decatur Dyspraxia editor’s notation.)
Key problems include:
- Difficulties controlling the speech organs.
- Difficulties making speech sounds
- Difficulty sequencing sounds
- Within a word
- Forming words into sentences
- Difficulty controlling breathing, suppressing salivation and phonation when talking or singing with lyrics.
- Slow language development
Diagnosis (high level overview)
Wikipedia: The American Psychiatric Association has four primary inclusive diagnostic criteria for determining if a child has developmental coordination disorder.
The criteria are as follows:
- Motor Coordination will be greatly reduced, although the intelligence of the child is normal for the age.
- The difficulties the child experiences with motor coordination or planning interfere with the child’s daily life.
- The difficulties with coordination are not due to any other medical condition
- If the child does also experience comorbidities, motor coordination is still disproportionally affected.
A MRI may be conducted to positively rule out any trauma or other non-dyspraxia related issues physical issues in the brain.
Now, before you panic, read what Dyspraxia is and what Dyspraxia is not.
